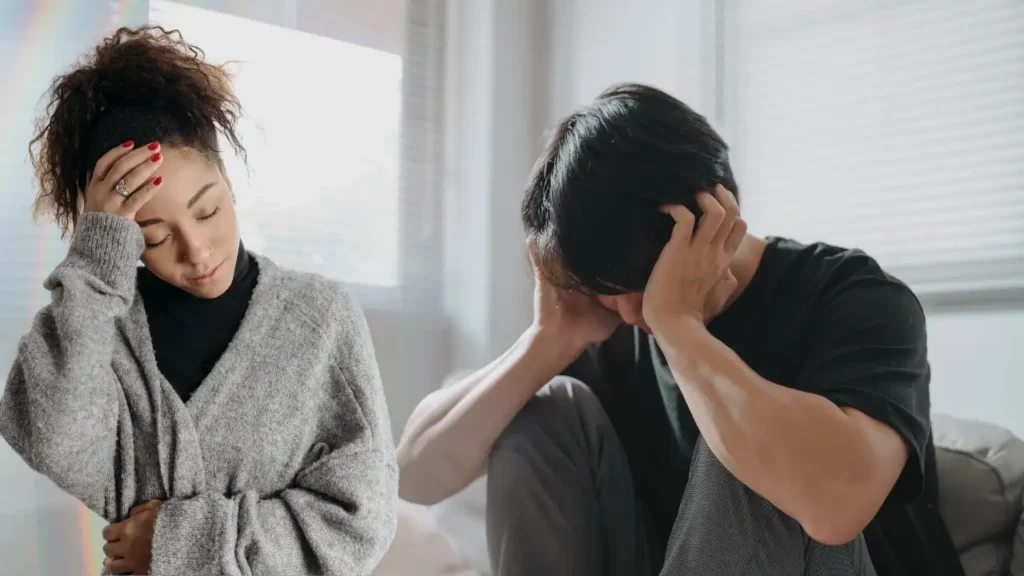
Introduction To Mental Health and Fever
The mind and body share a deep, interconnected relationship that many people often overlook. While it’s common to recognize the emotional impact of physical illness, the reverse is equally significant. Have you ever felt “sick” after a period of intense stress or emotional turmoil? Many of us have, but we might not realize how powerful our mental state is in shaping physical health. Understanding this connection is crucial not only for mental well-being but also for maintaining overall health. In this article, we’ll explore how emotions, particularly stress and anxiety, can manifest physically, sometimes even causing fever-like symptoms.
Understanding the Mind-Body Connection
The mind-body connection refers to the dynamic relationship between our thoughts, emotions, and physical health. This concept suggests that our mental state can directly influence bodily functions. For instance, when we experience stress or anxiety, our body responds by activating the sympathetic nervous system, often called the “fight or flight” response. This activation releases stress hormones like cortisol and adrenaline, which prepare the body to face perceived threats. However, when these stress responses become chronic, they can lead to various health issues, including headaches, digestive problems, and even fever-like symptoms.
Psychosomatic health is a term used to describe physical symptoms that arise from psychological factors. Unlike symptoms caused by infections or injuries, psychosomatic symptoms don’t have an obvious physical cause. Yet, they are very real and can significantly affect a person’s quality of life. Recognizing this connection can help us understand that taking care of our mental health is just as important as looking after our physical well-being.
What Is a Psychosomatic Fever?
A psychosomatic fever, also known as a stress-induced fever, occurs when emotional distress causes the body’s temperature to rise without an underlying infection. Unlike a traditional fever caused by bacteria or viruses, a psychosomatic fever is triggered by the body’s response to stress or intense emotional experiences. This type of fever usually manifests during periods of high anxiety, intense emotional strain, or even after traumatic events.
The physiological mechanism behind this involves the hypothalamus, the part of the brain that regulates body temperature. During stress, the hypothalamus can mistakenly signal the body to increase its temperature, mimicking the effects of an actual fever. This reaction is part of the body’s natural defense mechanism, but when it happens frequently, it can lead to persistent, unexplained fevers.
It’s important to differentiate between a true fever and a psychosomatic one. True fevers are typically accompanied by symptoms like chills, body aches, and a rapid increase in temperature. In contrast, psychosomatic fevers often present with milder symptoms and can fluctuate based on emotional states. Understanding these differences can help individuals seek the appropriate treatment, whether it’s medical or psychological.

The Science Behind Stress and Fever
The relationship between stress and fever is rooted in the body’s complex stress response system. When we encounter stressful situations, the hypothalamus—an integral part of the brain’s limbic system—activates the stress response. This activation leads to the release of cortisol, a hormone that helps regulate various bodily functions, including immune responses and inflammation.
Inflammatory markers play a key role in this process. When the body is under prolonged stress, it produces pro-inflammatory cytokines, which are proteins that regulate immune responses. An excess of these cytokines can lead to inflammation and even raise body temperature, mimicking fever-like symptoms. This is why some people experience fever or flu-like symptoms during periods of intense stress.
Research has shown that individuals with high-stress levels are more likely to experience physical symptoms, including fever. For example, a study published in the journal Psychosomatic Medicine found that people under chronic stress had higher levels of inflammatory markers and reported more frequent illnesses. These findings underscore the importance of managing stress not only for mental health but also for preventing physical ailments.
Common Emotional Triggers Leading to Physical Symptoms
- Several emotional triggers can lead to physical symptoms, including fever-like responses. Here are some of the most common:
- Anxiety
- Anxiety is one of the most prevalent emotional triggers. When someone experiences chronic anxiety, their body remains in a heightened state of alertness. This constant activation of the stress response can cause various physical symptoms, including increased heart rate, sweating, and even fever. Anxiety-related fevers are often low-grade but persistent and can worsen during periods of acute stress.
- Depression
- Depression doesn’t just affect mood; it also impacts physical health. People with depression often experience weakened immune systems, making them more susceptible to illnesses. Additionally, depression can lead to chronic inflammation, which is linked to fever-like symptoms. The connection between depression and physical health is a two-way street: poor physical health can exacerbate depression, and depression can lead to physical ailments.
- Stress
- Chronic stress is perhaps the most well-known trigger for physical symptoms. Stress activates the body’s fight-or-flight response, leading to the release of cortisol and other stress hormones. While this response is beneficial in short bursts, chronic stress can cause long-term health issues. One of these issues is stress-induced fever, where the body’s temperature rises as part of the stress response.
- Trauma and PTSD
- Individuals who have experienced trauma or suffer from post-traumatic stress disorder (PTSD) often report physical symptoms, including fever. Trauma can keep the body in a state of constant stress, leading to prolonged activation of the stress response system. This can result in various physical health problems, including unexplained fevers.

How Mental Health Issues Manifest as Physical Illness
Mental health challenges don’t just stay in the mind; they often spill over into physical well-being. The brain and body are deeply interconnected, and mental health issues can trigger physical responses. This connection is known as the psychosomatic effect, where psychological factors cause real, tangible physical symptoms. Let’s delve into how different mental health issues manifest physically:
Physical Conditions Linked to Mental Health
- Headaches and Migraines:
Stress and anxiety are common culprits behind tension headaches and migraines. The constant worry or overwhelming stress can cause muscles to tighten, particularly in the neck and scalp, leading to headaches. Studies show that individuals with chronic stress are more likely to suffer from frequent migraines. - Digestive Problems:
The gut is often called the “second brain” because it’s so sensitive to emotional states. Stress and anxiety can lead to digestive issues like irritable bowel syndrome (IBS), acid reflux, and even nausea. These conditions are exacerbated by prolonged stress, which affects the gut-brain axis. - Fever-like Symptoms:
When the body is under constant stress or emotional strain, it can mimic the signs of an infection, including fever. This is because the stress response involves the immune system and inflammatory pathways, which can raise body temperature.
The Role of Trauma and PTSD
Trauma has a profound impact on the body. People with PTSD often experience chronic stress, which keeps their bodies in a state of hyperarousal. This can lead to a variety of physical symptoms, such as muscle pain, fatigue, and fever-like responses. For many trauma survivors, these symptoms are a daily reminder of past experiences, adding to their emotional burden.

The Vicious Cycle Of Mental Health
There’s a feedback loop between mental health and physical health. For example, someone experiencing stress-induced fever might feel more anxious about their health, which, in turn, worsens the fever. Breaking this cycle often requires addressing both the mental and physical aspects simultaneously.
Signs Your Fever Might Be Emotion-Related
- Not all fevers are caused by infections. Sometimes, emotional distress is the underlying culprit. So, how can you tell if your fever is stress-induced? Here are some key indicators:
- Absence of Infection Symptoms:
- If you have a fever but no other signs of infection (like a sore throat, cough, or congestion), it might be psychosomatic. Stress-induced fevers usually don’t come with typical cold or flu symptoms.
- Fluctuating Temperature:
- Psychosomatic fevers often fluctuate throughout the day. They might spike during periods of high stress and decrease when you’re relaxed. In contrast, fevers caused by infections usually follow a more consistent pattern.
- Correlation with Emotional Events:
- If your fever tends to occur during stressful situations—like before an important presentation or after an emotional argument—it’s likely linked to your mental state.
- Relief with Relaxation Techniques:
- Stress-induced fevers often respond well to relaxation techniques. If your fever decreases after practicing mindfulness, deep breathing, or meditation, it’s a strong sign that stress is the trigger.
When to Seek Help:
- If you’re unsure whether your fever is stress-related or due to an underlying illness, it’s essential to consult a healthcare professional. They can rule out medical causes and, if necessary, refer you to a mental health specialist. Ignoring persistent symptoms can lead to more severe health issues, so it’s always better to err on the side of caution.
- The Impact of Chronic Stress on the Immune System
- Chronic stress isn’t just bad for your mood; it wreaks havoc on your immune system too. Here’s how it works:
- Weakened Immune Response:
- When you’re stressed, your body produces cortisol. While cortisol is helpful in short bursts, chronic stress keeps cortisol levels high, which can suppress the immune system. This makes you more susceptible to infections and illnesses.
- Increased Inflammation:
- Stress triggers the release of pro-inflammatory cytokines. While these proteins are essential for fighting infections, an overabundance can lead to chronic inflammation, which is linked to various health problems, including heart disease, diabetes, and autoimmune disorders.
- Susceptibility to Illness:
- People under chronic stress are more likely to get sick. This is because their bodies are constantly in “fight or flight” mode, diverting resources away from the immune system. Over time, this leaves them vulnerable to infections.
- Effects of Burnout:
- Burnout is the result of prolonged, unrelenting stress. It doesn’t just affect your mental state; it can cause physical symptoms like fatigue, headaches, and even fever. Recognizing the signs of burnout early can help you take steps to protect both your mental and physical health.
Mental Health Disorders and Their Physical Correlates
Mental health disorders don’t just affect the mind—they leave a mark on the body too. Various mental health conditions manifest physically, and understanding these connections can help in addressing both aspects of well-being. Let’s look at some common mental health disorders and their physical correlates:
Anxiety Disorders:
Anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, and social anxiety, are often accompanied by physical symptoms. These can include:
- Rapid heartbeat: Anxiety triggers the body’s “fight or flight” response, leading to palpitations or an elevated heart rate.
- Shortness of breath: Panic attacks can cause hyperventilation, making it feel difficult to breathe.
- Muscle tension: Chronic anxiety leads to muscle stiffness, especially in the neck, shoulders, and back.
- Fever-like sensations: Anxiety can elevate body temperature, causing sweating and chills that mimic a fever.
2. Depression
Depression goes beyond feelings of sadness and can affect physical health in profound ways:
- Fatigue and lethargy: People with depression often experience low energy levels, which can make even simple tasks feel exhausting.
- Sleep disturbances: Both insomnia and hypersomnia are common in depression, disrupting the body’s natural rhythms.
- Lowered immunity: Depression weakens the immune system, making the body more vulnerable to infections.
- Chronic pain: Persistent aches and pains are common, particularly in the back or joints.
3. Panic Disorders
Panic attacks are intense episodes of fear or anxiety that come on suddenly and peak within minutes. They often include physical symptoms such as:
- Chest pain: This can be mistaken for a heart attack, adding to the panic.
- Sweating and shaking: The body’s response to fear leads to these visible signs.
- Feeling feverish: Many people report feeling overheated or chilled during a panic attack, similar to having a fever.
4. Post-Traumatic Stress Disorder (PTSD)
PTSD develops after experiencing or witnessing a traumatic event. Its physical symptoms include:
- Hyperarousal: Constantly feeling on edge can lead to an increased heart rate and heightened reflexes.
- Sleep problems: Nightmares and insomnia are common in PTSD, which can lead to fatigue and irritability.
- Physical pain: Many individuals with PTSD experience chronic pain, headaches, and digestive issues.
Coping Mechanisms to Manage Emotional Health and Reduce Physical Symptoms
Managing emotional health is crucial not only for mental well-being but also for preventing physical symptoms like fever. Here are some effective coping mechanisms:
1. Stress Management Techniques
- Mindfulness and Meditation: Practicing mindfulness helps you stay present and reduces stress levels. Even a few minutes of deep breathing can calm the nervous system.
- Progressive Muscle Relaxation (PMR): This involves tensing and relaxing different muscle groups, which helps release physical tension.
- Journaling: Writing down your thoughts and feelings can provide an emotional release, reducing stress.
2. Lifestyle Changes for Better Mental Health
- Regular Exercise: Physical activity boosts endorphins, which are natural mood elevators. Exercise also helps reduce cortisol levels.
- Healthy Diet: Foods rich in omega-3 fatty acids, such as fish, flaxseeds, and walnuts, can support brain health. Avoiding caffeine and sugar can help prevent anxiety spikes.
- Adequate Sleep: Establishing a regular sleep schedule is essential for mental and physical health. Poor sleep exacerbates stress and weakens the immune system.
3. Importance of Therapy and Counseling
- Cognitive Behavioral Therapy (CBT): CBT is one of the most effective treatments for managing stress, anxiety, and depression. It helps individuals identify and change negative thought patterns.
- Talk Therapy: Sometimes, simply talking to someone can lighten the emotional load. Professional counselors can offer strategies for coping with stress and reducing its physical impact.
4. Building a Support System
- Social Connections: Surrounding yourself with supportive friends and family members provides a buffer against stress. Talking to someone who understands can make a world of difference.
- Support Groups: Joining a support group for people facing similar challenges can be comforting and empowering.
When Should You See a Doctor?
- Determining whether your physical symptoms are due to stress or an underlying medical condition can be challenging. Here’s when to seek professional help:
- 1. Persistent Symptoms:
- If you’ve tried managing stress and your symptoms persist, it’s essential to consult a healthcare provider. Persistent fever, chronic pain, or severe fatigue needs evaluation to rule out medical causes.
- 2. Severe Physical Reactions:
- If you experience severe symptoms, such as chest pain or difficulty breathing, seek immediate medical attention. These could indicate a serious condition, even if stress is a contributing factor.
- 3. Emotional Health Concerns:
- If stress, anxiety, or depression is interfering with your daily life, reaching out to a mental health professional is crucial. They can provide coping strategies and, if necessary, recommend medication.
- 4. Holistic Approach:
- Many healthcare providers now take a holistic approach, addressing both physical and mental health. Don’t hesitate to discuss your emotional well-being with your doctor—they’re there to help with the whole picture.
The Role of Healthcare Providers in Recognizing Emotional Health Impacts
Healthcare providers play a crucial role in identifying and addressing the physical manifestations of mental health issues. Here’s how they contribute:
- 1. Holistic Assessments
- Many doctors are now adopting a holistic approach, considering both physical and emotional factors when diagnosing symptoms. They may ask about stress levels, recent life events, and overall mental well-being to get a complete picture.
- 2. Collaboration Between Disciplines
- Effective treatment often involves collaboration between different healthcare professionals. For instance, a general practitioner might work alongside a psychologist or psychiatrist to address both the physical and mental aspects of a patient’s condition.
- 3. Education and Awareness
- Healthcare providers can educate patients about the mind-body connection, helping them recognize how their emotional state might be affecting their physical health. This awareness empowers patients to take a proactive approach to managing stress and seeking help when needed.
- 4. Integrative Therapies
- Some healthcare providers recommend integrative therapies, such as yoga, acupuncture, and biofeedback, to help patients manage stress. These therapies can complement traditional treatments and provide a more comprehensive approach to health.
Self-Care Strategies for Maintaining Emotional and Physical Health
Maintaining both emotional and physical health requires a proactive approach. Here are some self-care strategies that can help you stay balanced:
1. Practice Mindfulness and Meditation
Mindfulness involves staying present and fully engaging with the current moment. Meditation helps calm the mind and reduce stress. Even 10 minutes of daily meditation can have a significant impact on your emotional well-being.
2. Establish a Routine
A structured daily routine provides stability and reduces uncertainty, which can help lower stress levels. Include time for relaxation, exercise, and hobbies that bring you joy.
3. Engage in Regular Physical Activity
Exercise is a powerful stress reliever. It releases endorphins, which are natural mood boosters. Aim for at least 30 minutes of moderate exercise most days of the week.
4. Prioritize Sleep
Quality sleep is essential for both mental and physical health. Aim for 7-9 hours of sleep each night. Establishing a consistent sleep schedule and creating a calming bedtime routine can improve sleep quality.
5. Build a Support Network
Surround yourself with supportive friends and family members. Talking to someone you trust can help you process emotions and reduce stress. Don’t hesitate to seek professional support if needed.
6. Practice Healthy Eating Habits
A balanced diet rich in whole foods supports overall well-being. Avoid excessive caffeine, sugar, and processed foods, as they can contribute to anxiety and mood swings. Include plenty of fruits, vegetables, lean proteins, and healthy fats in your diet.
7. Engage in Relaxing Activities
Find activities that help you unwind, such as reading, listening to music, gardening, or spending time in nature. These activities can provide a much-needed break from daily stressors.
8. Set Realistic Goals
Setting achievable goals and breaking them down into manageable steps can prevent feelings of overwhelm. Celebrate small victories along the way to stay motivated.
Conclusion
The connection between mental health and physical symptoms, such as fever, is undeniable. Emotions, particularly stress and anxiety, can manifest physically in various ways, including fever-like sensations. Understanding this mind-body relationship is crucial for managing both mental and physical health. By recognizing the signs of stress-induced symptoms and adopting effective coping strategies, you can take control of your well-being. Remember, seeking professional help is not a sign of weakness but a step toward holistic health.
FAQs
1. Can stress cause a real fever?
Yes, stress can cause a psychosomatic fever. Emotional distress can activate the hypothalamus, which regulates body temperature, leading to fever-like symptoms without an underlying infection.
2. How do I know if my fever is stress-related?
If your fever occurs during periods of high stress and is not accompanied by typical infection symptoms (like a sore throat or cough), it might be stress-induced. Relaxation techniques that reduce the fever also suggest a stress connection.
3. What should I do if I think my emotions are making me sick?
Start by practicing stress management techniques, such as mindfulness, meditation, and regular exercise. If symptoms persist, consult a healthcare professional to rule out other causes and consider talking to a mental health specialist.
4. Are certain mental health conditions more likely to cause physical symptoms?
Yes, conditions like anxiety, depression, and PTSD are often associated with physical symptoms, including headaches, digestive issues, and fever-like sensations. Managing these conditions can help alleviate physical symptoms.
5. Can therapy help with physical symptoms caused by stress?
Absolutely. Therapy, particularly cognitive-behavioral therapy (CBT), can help you manage stress and anxiety, reducing their physical impact. Therapists can provide coping strategies and support to improve both mental and physical health.
Follow us on Facebook
Read This Also: Are You Making This Common Mistake with Nutrition Drinks?, How Do You Build Muscle With High Metabolism?